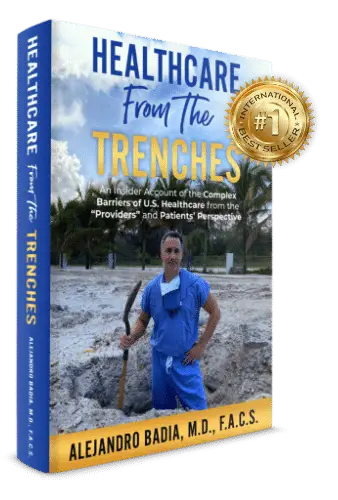

"IT’S TIME FOR EVERY AMERICAN TO UNDERSTAND AND BE EDUCATED ABOUT THE ROOT CAUSES OF OUR HEALTHCARE CRISIS AND DEMAND MEANINGFUL REFORM"
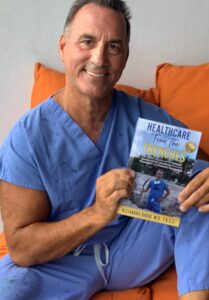
Dr. Alejandro Badia
Americans are facing serious problems – skyrocketing healthcare costs, a lack of patient access, and inefficient delivery. Now with the frightening COVID-19 pandemic that is further taxing our healthcare system – and our economy – these issues are amplified. Despite all the political debates and media coverage on healthcare policy and reform, there is always one glaring omission: feedback from the people in the trenches – the doctors and other healthcare professionals who provide care to the patients.

Americans are facing serious problems – skyrocketing healthcare costs, a lack of patient access, and inefficient delivery. Now with the frightening COVID-19 pandemic that is further taxing our healthcare system – and our economy – these issues are amplified. Despite all the political debates and media coverage on healthcare policy and reform, there is always one glaring omission: feedback from the people in the trenches – the doctors and other healthcare professionals who provide care to the patients.


Monday- Friday: 8:30AM- 5:00 PM
Saturday- Sunday: Closed